I have learned over the years that doctors who are digital natives, or at least comfortable with the technologies that I use (email and the web), are those doctors that I want to treat me. In the past, whenever I have looked for treatment, I have followed a different path to choose my doctor, looking for someone who was older with loads of experience, who has seen plenty of patients.
But older experience isn’t necessarily relevant anymore, and as I age that is also pushing the envelope of what “older” really means. The older docs got their medical education more than 30 years ago, when there were different treatment modalities, different standards of medical care, and computers were the size of rooms. This is why I went with my urologist, someone closer to my kids’ age than mine, when two years ago I had my prostate removed surgically. The operation went well, and was done with the DaVinici robotic device made by Intuitive Surgical. My surgeon, Eric Kim, did touch me during the surgery — to open and close me up and position the robotic arm The rest of the time he was using the robot.
The robots have some big advantages over manual methods. Patients spend less time in the operating room, not to mention a reduction in blood loss, much smaller incisions and shorter hospital stays. Kim estimates that less than five percent of all prostates are removed by manual methods anymore. He has done more than 100 surgeries using the latest model of the daVinci, one that requires a single incision. Many of his patients that had surgery with this model of the robot — myself included — were able to go home within a few hours.
The robots have another direct benefit: “The doctor has instant feedback from an ultrasound or heart-lung machine without taking their eyes off of the procedure and operating field in progress,” said David Powell, the principal design engineer for Intuitive.
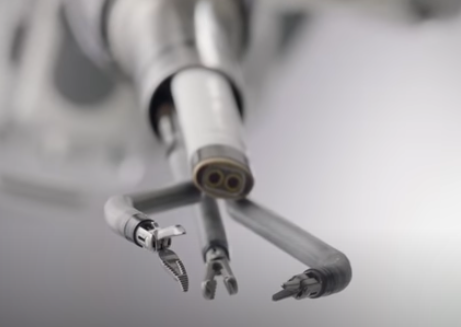 Being interested in technology, I have learned that these robots have evolved from using 3D standard-definition stereo vision to today’s dual-console, multi-window 3D high-definition systems. These units can be found in hundreds of hospitals around the world and are used to perform numerous urology, thoracic, ENT and gynecologic laparoscopic surgical procedures.
Being interested in technology, I have learned that these robots have evolved from using 3D standard-definition stereo vision to today’s dual-console, multi-window 3D high-definition systems. These units can be found in hundreds of hospitals around the world and are used to perform numerous urology, thoracic, ENT and gynecologic laparoscopic surgical procedures.
The company has worked with Xilinx for two decades, upgrading their Virtex and Spartan FPGA video processing chipsets to make the views seen by their human surgeons more helpful and more precise. Plus, the better video setup means less eye strain for the surgeon, and the ability to train new staff members.
“Xilinx’ embedded processor architecture has led to a major revolution for us in terms of our subsequent platform designs,” said Powell. The current daVinci models employ dozens of these chipsets, and benefits from being programmable, as well as a more scalable and distributed architecture. This means that many new capabilities can be introduced with an in-field firmware upgrade, rather than swapping out major hardware components. All of this results in more uptime and increased robot usage, amortizing their costs over more surgeries. Our hospital has seven of the machines — both older and newer models — that are busy at most times. “It is rare for a robot to sit unused,” said Kim.
It is easy to recognize the newer electronics, because the original daVinci models used a collection of thick custom cables to connect its various components that were failure-prone and required frequent repairs. The current version uses a single fiber optic line to deliver eight channels of full 1080i HD video and is more reliable. Sadly, I wasn’t able to see the machine that did the deed on my prostate, but glad that I got the benefits!
David, that’s very interesting why you prefer younger surgeons who are more familiar with medical technology. There’s another reason to prefer younger doctors. My mother, a very smart woman who is now gone, told me that a downside of experience is overconfidence, a disinclination to recognize one’s mistakes or gaps in knowledge. A doctor’s tendency to jump to conclusions based on what they have already seen can be deadly when your particular case is the exception. Of course it is natural to make assumptions based on previous experience and if we didn’t do that, we could hardly get through the day. But we, all of us including doctors, can take that too far
When I was having cataract surgery I opted for robotic incision, destruction and removal of the existing lenses. I trusted the robot more than my doctor’s own hands. And I have “complicated” eyes, after two serious retinal tears repaired by lasers. That was in Covid 2020 just after hospitals opened back up for general patient surgeries. A number of my friends who have had cataract surgery have had to go back for more laser work because of “cloudiness.” I’ve read that this is often because the original lens wasn’t destroyed and/or removed. Knock on wood… I’ve not had that problem… at least not yet. Here’s hoping the robot was the right choice.